Fetal medicine
Clinical case
Publié le 15 May 2019Lecture 8 min
Diagnosis and management of complex cardiac malformation : comparison of approach between centers of France and India
Viral PANDYA1,2, Vijay PATIl3, Philippe ROTH1, Marilyne LEVY4, Maryse BONNIERE5, 1. Service d’Obstétrique-maternité, chirurgie médecine et imagerie foetale, Hôpital Necker Enfants Malades, Paris, France ; 2. Kanan Maternity and Nursing
We present here two clinical cases of fetal heart malformations diagnosed during second trimester of pregnancy.
Case 1 : Mrs X., aged 21, India
A twenty-one years old primigravida patient Mrs X. was referred for second trimester anomaly screening scan at 19 + 2 weeks of gestational age.
Ultrasound findings and diagnosis
On ultrasound assessment, fetal growth was found corresponding to gestational age. On fetal cardiac screening sections, abnormalities were suspected. Further detailed echocardiography, including Doppler flow analysis and STIC imaging was conducted.
Findings of fetal echocardiography:
1. Single outflow tract noted, arising from both ventricles;
2. Common truncal valve in outflow tract;
3. Small perimembranous VSD;
4. Intact muscular part of intraventricular septum;
5. No distinct pulmonary trunk;
6. Both pulmonary arteries noted to be arising from the posterior aspect of the common trunk;
7. Hypoplasia of thymus.
Additional findings on detailed ultrasound study:
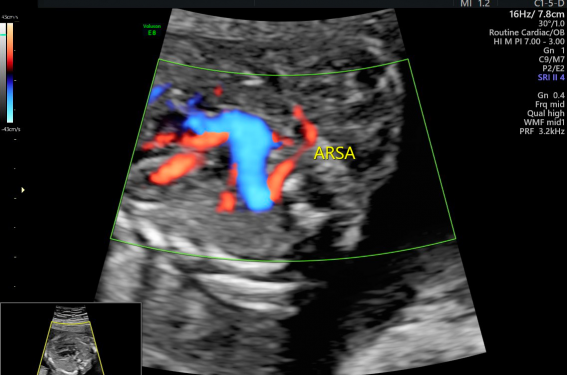
1. Aberrant right subclavian artery – marker for numerical chromosomal abnormalities;
2. Isolated pelvic cysts, two in number, largest diameter 7.8 mm – possibly mesenteric cysts.
The final diagnosis was noted to be Common arterial trunk, type II(1), with thymic hypoplasia and aberrant right subclavian artery. Associated findings included the presence of two mesenteric cysts in the pelvis.
Counselling
The couple was counselled regarding the condition and the high association with genetic and chromosomal abnormalities (4:100 for trisomy, 1:3 for 22q11 microdeletion)(1).
Information was given regarding the various management options and prognosis, including the prospect of multiple corrective surgeries during infancy, to restore normal cardiac physiology.
As the pregnancy was still within the legal termination limit of 20 weeks gestational age, medical termination of pregnancy was also offered as an option(2).
Management
Patient opted for prenatal testing for genetic abnormalities. An amniocentesis was performed under strict aseptic precautions, and amniotic fluid was sent for rapid fluorescence in-situ hybridization assay for numeric chromosomal abnormalities and 22q11 microdeletion.
The FISH report returned positive for 22q11 microdeletion. The couple was informed about the outcome of the investigation, and they opted for termination of the pregnancy.
Pregnancy was terminated according to the local protocols. The couple did not opt for autopsy examination of the fetus, or further familial genetic testing due to financial constraints.
Case 2 : Mrs Y. aged 29 years, France
A twenty-nine years old primigravida patient, Mrs Y. was referred for second trimester anomaly screening scan at 24 + 3 weeks gestational age.
Ultrasound findings and diagnosis
First trimester ultrasound assessment was not suggestive of any abnormalities. The screening risk for T21 was 1:3000.
On second trimester ultrasound at 22 weeks, fetal growth was corresponding to gestational age. On fetal cardiac screening sections, abnormalities were suspected and the patient was referred to tertiary center at Hôpital Necker.
At Necker, primary scanning was done at 23 + 4 weeks gestational age in the Diagnostic AnteNatal (DAN) service. The patient was also referred for a same day scanning appointment to PARSIFAL service for expert cardiac assessment. Further detailed echocardiography, including Doppler flow analysis was conducted at UE3C.
Findings of fetal echocardiography:
1. Pulmonary atresia;
2. Intact ventricular septum;
3. Smaller cavity size of right ventricle, with hypertrophy of ventricular wall;
4. Tricuspid insufficiency;
5. Atretic pulmonary valve;
6. On Doppler assessment, reverse flow in pulmonary artery (from DA).
The final diagnosis was noted to be pulmonary atresia with intact ventricular septum (PA-IVS), associated with tricuspid insufficiency and deformed right ventricle (small cavity, hypertrophic wall).
Counselling
The couple was counselled regarding the guarded prognosis of the condition, especially in the presence of smaller right ventricle cavity and tricuspid insufficiency, which are markers for poor postnatal outcome(1). The couple was informed that genetic and chromosomal abnormalities (trisomies, 22q11 deletion) are rarely noted with PA – IVS(1).
Information was given regarding the various management options and prognosis, including the prospect of surgical intervention (pulmonary valve perforation, balloon dilatation), to restore normal cardiac physiology(1).
As per the legal status of termination in the country, medical termination of pregnancy was also offered as an option(3).
Management
With the consent of the couple, an amniocentesis was performed under strict aseptic precautions, and amniotic fluid was sent for array CGH analysis and florescence in-situ hybridization assay.
The couple opted for termination of the pregnancy. Termination was carried out according to the local protocols. The fetus was further assessed by autopsy examination by the fetopathology team.
Autopsy Findings
The autopsy noted a fetus consistent in measurements of size with the gestational age of 25 + 4 weeks at termination.
The morphological findings at autopsy were as follows:
1. Thin lips, excess of skin at nape of neck, short and bulging philtrum;
2. Pulmonary artery was smaller than aorta;
3. Hypoplastic cavity of the right ventricle, with hypertrophy of ventricular wall and subendocardial fibrosis on histopathological examination;
4. Atretic pulmonary valve with fusion of pulmonary valve leaflets;
5. Asymmetry of cerebral hemispheres;
6. Enlargement of cerebral right ventricle;
7. Choroid plexus cyst at the level of foramen of Munro.
Genetic Analysis
The array CGH report noted a deletion of 1.2 Mb size at 1q21.1q21.2. Deletion in this region has incomplete penetrance and is associated with heart disease and intellectual disability(4).
Further familial genetic testing was carried out. Similar deletion was noted in the mother and sibling of mother. However, neither of the individuals present any abnormalities as a result of this deletion.
Discussion and comparison of differences
The contrast between the approaches to the management of the two cases illustrates the fundamental difference of infrastructure and legal maneuverability between the developed and the developing world.
► In India, the public health system is vastly understaffed and underdeveloped. The majority of the population is reliant on private healthcare, especially for specialized consultations like fetal medicine or genetics. The prohibitively high costs for diagnostic evaluation makes affordability a key factor in the decision making of the couples. In such a scenario, expensive investigations like array CGH, familial genetic testing or fetal autopsy are but a luxury which the majority of the population cannot afford.
France has a very well established public health system. The mandatory subscription to social security covers all financial expenses of pregnancy care. Thus the monetary cost becomes a non-existent factor in decision-making.
► There is a dearth of well-trained specialists in fields like fetal cardiology, fetal MRI, fetal surgery, clinical genetics and fetopathology. This has resulted in compromised quality of healthcare, and increase in the number of terminations in cases that could have been managed otherwise in a well-equipped center or country.
Established referral protocols, and the availability of highly skilled specialists at tertiary centers, streamline the process of obtaining an expert opinion. Many complex conditions that would otherwise be considered non-salvageable, can be managed with significantly good outcomes due to the level of expert care available.
► The Medical Termination of Pregnancy Act(2) establishes a legal limit of 20 weeks of gestational age beyond which termination of pregnancy is illegal in India. This often becomes a challenge for fetal medicine specialists, as many fetal anomalies are difficult to diagnose before 22-24 weeks. Hence, early diagnosis of fatal abnormalities has become the primary area of focus.
Under the French Law on Voluntary Termination 79-1204(3), a pregnancy can be terminated at any stage if two panel-approved specialists certify that termination is necessary due to the possibility of serious permanent injury to the physical or mental health or risk to the life of the pregnant woman, or that the child will suffer from a particularly severe illness recognized as incurable. This provision enables fetal care physicians to carry out appropriate investigations before making decisions regarding termination of the pregnancy. Certain investigations like MRI give better results if done after 24 weeks. Genetic testing like array CGH or next-generation sequencing may take a few weeks for the results to be established. As there is no time-bound limitation for termination, the patient and the treating specialists are able to make well-informed decisions regarding the progress of the pregnancy.
► The focus on early diagnosis, and the relative unavailability of MR imaging, has resulted in increased dependence on high-quality ultrasound. This has resulted in the Indian fetal medicine specialists being highly skilled in obstetric ultrasound. Use of advanced 3D imaging, STIC imaging for cardiac defects and high-resolution intracavitary scanning became mainstream in most fetal medicine centers across India.
Contrastingly, the area of focus is completely different for developed countries. The liberal use of MR imaging, and use of cutting-edge, experimental technologies like bone scanning are complementary to ultrasonography. This enables the consultants to counsel the patient more efficiently. The availability of advanced genetic testing facilities also contributes to research and discovery of novel genetic abnormalities.
Thus the approach to the case is adapted to the specific needs and limitations of the concerned population. This comparative case report demonstrates that this adaptation can be achieved whilst staying within the purview of the peer-reviewed management guidelines.
In the Indian scenario, there exist limitations for the use of expensive technology for diagnostic aid. This, coupled with the early limit for termination, and the high patient-to-specialist ratio, has resulted in the development of a diagnostic setup highly reliant on clinical diagnosis aided by high-quality imaging using a single, most affordable modality, which is ultrasound in majority of the centers.
Meanwhile, in France, advanced investigative tools and multimodal fetal imaging (ultrasound, MRI, CT) help share the burden of proof with clinical diagnosis. This added information can help the specialist to reconfirm the diagnosis, and the patient can be counselled appropriately to make a well-informed decision. Due to the relatively well-established protocols and the availability of diagnosis and follow-up data throughout the health system, the specialist can also use his clinical and scientific acumen to study and analyze patterns. The academic and research pursuits help to improve the management and enhance the outcomes.
Vidéo 1 : This clip demonstrates a sweep through the fetal heart, where we can note the intact muscular intraventricular septum, peri-membranous VSD with override of the single outflow tract, two vessels in the 3VV and hypoplastic thymus.
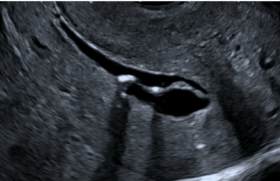
Figure 2 : 2D image demonstrating presence of two vessels – common truncus and superior vena cava, in the 3VV.
Figure 3 : Color Doppler flow imaging of the cardiac chambers during fetal diastole, demonstrating adequate filling of ventricles across the atrio-ventricular valves, and an intact muscular portion of the intraventricular septum.
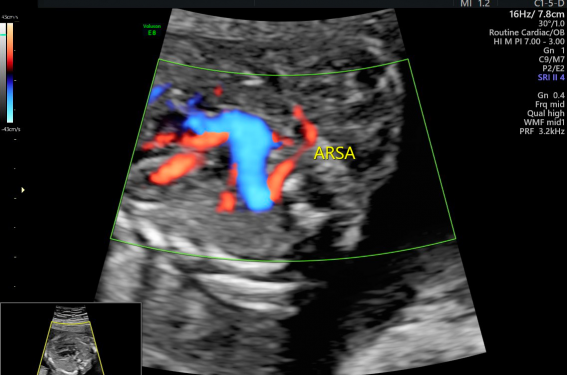
Figure 4 : Color Doppler flow imaging demonstrating the aberrant right subclavian artery, arising from the common trunk and arching behind the trachea towards the right side shoulder of the fetus.
Figure 5 : STIC rendering of cardiac blood flow, visualized from the posterior aspect. Note the origins of the right and left pulmonary arteries from the common trunk. The ARSA is also demonstrated.
Vidéo 2 : Clip demonstrating the STIC rendering of the cardiac defect – common arterial trunk with ARSA.
Figure 7 : Laboratory report from amniotic fluid analysis by fluorescence in-situ hybridization, demonstrating deletion of locus 22q11.
Vidéo 3 : 2D clip which demonstrates the hypertrophic wall and the small cavity of right ventricle. Note the intact ventricular septum.
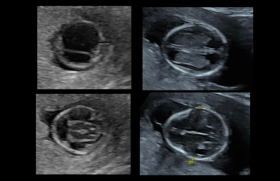
Figure 9 : The incompliant tricuspid valve, compared to the competent mitral valve, seen during diastole.
Vidéo 4 : This clip demonstrates the reversal of blood flow through the ductus arteriosus into the atretic pulmonary artery.
Figure 11 : This still image demonstrates the reversal of blood flow through the ductus arteriosus into the atretic pulmonary artery.
Figure 12 : Autopsy confirmed the right ventricular findings – hypertrophy of wall, with a small cavity.
Figure 13 : This image demonstrates the caliber difference of the great vessels – aorta and pulmonary artery.
Figure 14 : Fusion of valve flaps of the pulmonary valve.
Figure 15 : Histological examination of right ventricular wall shows subendocardial fibrosis.
Figure 16 : The cerebral hemispheres are visibly discrepant in size.
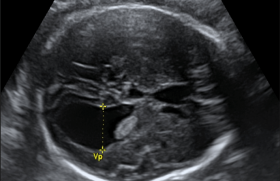
Figure 17 : Coronal section of the cerebral hemispheres, illustrates unilateral ventriculomegaly on the right side.
Figure 18 : Microscopic examination demonstrates the presence of choroid plexus cyst at the level of foramen of Munro in the cerebral ventricular system.
Figure 19 : Laboratory report from amniotic fluid analysis by array comparative genomic hybridization, demonstrating deletion in the 1q21 region.
Attention, pour des raisons réglementaires ce site est réservé aux professionnels de santé.
pour voir la suite, inscrivez-vous gratuitement.
Si vous êtes déjà inscrit,
connectez vous :
Si vous n'êtes pas encore inscrit au site,
inscrivez-vous gratuitement :